
My Massage recommendations, in a nutshell:
Set aside 5 minutes, twice daily, to work on massaging the area.
Use your hands/fingers/palms, this will help control the hardness/pressure
Rub the area with moderate pressure. Moderate pressure should indent the skin to reach the lower sections but not be painful.
Rub in circular fashion. Try to move the skin and slide the skin back and forth (massage guns and rollers do not do this well, only a hand can). This is the step to promote tissue mobility
Move your hand around to target all the surgical areas
You may spend a bit more time on harder areas
Repeating twice daily, a period of 2 months is perfect.
Introduction:
one of the most common questions I get is regarding need and timing of massage after gynecomastia surgery. In this page, I will summarize my thoughts on what the goals should be, what I feel the mechanism of improvement is, and what things to avoid.
One word, many meanings:
We speak of massage, but it is just one word, with different techniques that patients undertake, from self gentle massage, to “massage guns”, and finally to professional massages. Massage differs from patient to patient in terms of pressure applied, hardness of object used (massage guns /rollers vs hands), duration of treatment, and frequency of treatment.
Therefore, in addition to when to massage, we need to figure out what intensity and technique to use.
Is there such a thing as too much or too hard?
A misconception is that massage can’t hurt and may help. Unfortunately, that is not true.
When I am dealing with gynecomastia patients,, the patient has been bothered and affected for years on the appearance of their chest. Surgery is such large expense and such a relief that the patient feels they might as well go all in to ensure best results and best outcomes. So sometimes they feel less is more, and do much more aggressive massages than is recommended.
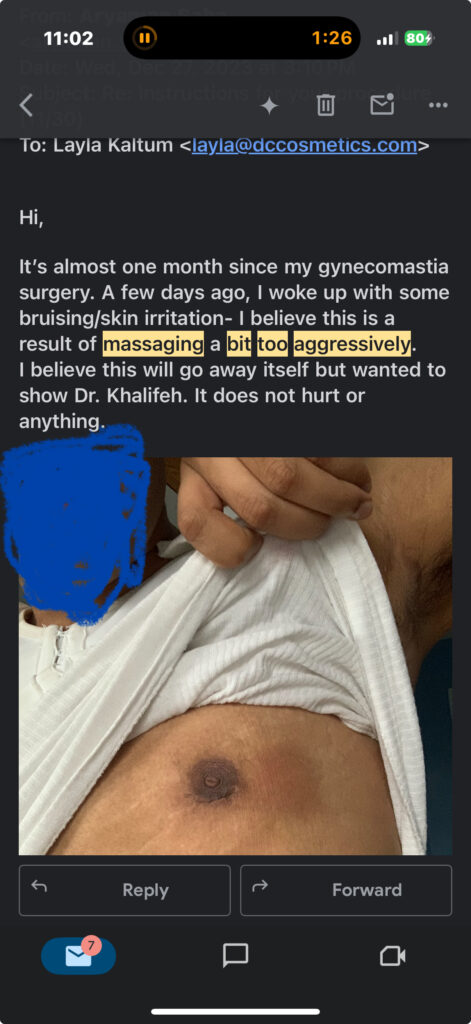
Below is an example of an email I will on occasion get from an overzealous patient. Note the new bruising around the areola where he was trying to “work” off scar tissue. Fortunately, this resolved without permanent issues, but it could have led to tissue disruption/fat necrosis. He was doing great prior to starting his “massage gun” sessions that he read about on the internet.
What is happening to tissues? And what is the theory behind massaging.
Post surgery I feel there are three types of processes that need help:
Why I feel my surgical technique has less trauma and requires less vigorous massaging:
Every surgeon has different techniques.
My surgical technique has two elements that I have migrated to over the years that enhance the results, and with the same mechanism, reduce the need to massage via the same mechanisms, and they are as follows
B) Because I do quilting sutures, or sutures that reattach the overlying skin back to the muscle and help me position the fat where I wanted, there is less potential space for fluid and blood to accumulate in the immediate postop period. This leads to less massage needs
Goals of massaging:
My Massage recommendations, in a nutshell:
Set aside 5 minutes, twice daily, to work on massaging the area.
Use your hands/fingers/palms, this will help control the hardness/pressure
Rub the area with moderate pressure. Moderate pressure should indent the skin to reach the lower sections but not be painful.
Rub in circular fashion. Try to move the skin and slide the skin back and forth (massage guns and rollers do not do this well, only a hand can). This is the step to promote tissue mobility
Move your hand around to target all the surgical areas
You may spend a bit more time on harder areas
Repeating daily, a period of 2 months is perfect.